Summary
The number of children susceptible to measles in Aotearoa New Zealand (NZ) is growing. We are close to the number that triggered previous measles epidemics here. Alongside improving infant immunisation coverage, we urge three immediate actions to prevent another epidemic.
First, catch-up MMR immunisation for those aged 15 months to 9 years without documented receipt of two doses of MMR vaccine. Priority should be given to existing immunisation requirements for primary schools and pre-schools to reach a 95% plus coverage target. It is these institutions that particularly drive spread in the community.
Second, improved communication to travellers about measles risk. For residents even more than visitors, as those returning home are more likely to import the virus.
Third, to rethink our response to new measles cases arising in the community to have a stronger immunisation component.
The global increase in measles cases has set off alarm bells and warnings of a nation-wide measles epidemic in Aotearoa New Zealand (NZ).1 With latest immunisation coverage at age two years at around 80%—well short of the 95% target—the number of measles-susceptible children increases by around 1000 every month.
In this Briefing, we estimate the number of susceptible children in 2024 which shows how close we are to a nation-wide epidemic of the scale last seen in 1991.
Predicting and preventing measles epidemics
In 1997, a national MMR immunisation campaign for all children aged 2-10 years was planned from July, to close the immunity gap identified in that cohort.2 But the epidemic had started by April 1997. The belated immunisation campaign still prevented an estimated 90-95% of expected cases.3
Subsequent immunisation coverage improvements and lowering the age of the second MMR dose meant that it was the last nation-wide epidemic. The World Health Organization (WHO) certified measles elimination in NZ in 2017. Although the 2019 measles epidemic was the largest since 1997, high immunity in primary schools limited spread (see Appendix 1 for more details of this and other epidemics since 1997).
But immunisation coverage has been falling from 2017. In Appendix 1, we calculate the number of susceptible children and compare this to the epidemic threshold we observed in 1996—about 130,000 susceptible children. As of 2024, we estimate at least 156,000 susceptible children aged under 17 years, of whom over 117,000 are aged under 12 years.
In addition, we now have more adults who are susceptible than in 1997 (see Appendix 1). The number of susceptible people and the loss of high immunity in primary schools imply a large measles epidemic risk with consequences for the health sector; and those made miserable, disabled or dead.
Actions to prevent the next measles epidemic
We suggest three urgent actions to prevent a measles epidemic from occurring, while we continue to focus on improving infant coverage – the most important measure to prevent creating future immunity gaps. These measures build on those outlined in our February Briefing.1
1. Close the immunity gap
Closing the immunity gap for those born from 2016 is the highest priority to prevent a measles epidemic. Primary schools and ECCs are the key settings of epidemic spread. This is one reason that the Health (Immunisation) Regulations 1995 requires service providers to keep an Immunisation Register. This institutional requirement provides a mechanism to identify unvaccinated children to offer them immunisation.
We need joint action from Health and Education Ministries to implement policies and processes to comply with the Immunisation Regulations and to achieve 95% coverage targets in all primary schools and ECCs, starting with those in urban areas and serving deprived communities.
The keeping of immunisation registers has been variable, with minimal resources or attention. Bringing the registers up to date makes it easier to identify susceptible individuals in an outbreak.
While the task is simple, it does require staffing for each school/ECC to (1) identify those who are not vaccinated; (2) sensitively engage and address concerns of vaccine-hesitant parents; and (3) vaccinate.
One option for staff resourcing is to defer the HPV vaccine second dose to liberate Public Health Nursing time. Evidence of the effectiveness of one dose led WHO to recommend a one-dose schedule in 2022.4 Several countries, including Australia and England, moved to a one-dose HPV schedule in 2023.
2. Reduce the risk of importing measles
Immediate government action can reduce the risk of importing measles virus. Requiring measles immunity documentation to leave or enter NZ raises legal and other challenges, but its feasibility could be rapidly evaluated.
Meanwhile, the need for measles immunity can be communicated through existing systems, including regular media releases to highlight the risks of measles. Current official advice for travellers is limited to a reminder to “ensure that all your routine immunisations are up-to-date.” It does not highlight the growing international measles risk, and the risk of travellers bringing virus home to NZ. We offer suggestions in Appendix 2 and consider other border measures.
3. Rethink our response to measles cases
The public health response to measles cases focusses on identifying and isolating contacts. Susceptible contacts are offered MMR vaccine but only if this can be given within three days of their last exposure to the case and mostly contacts are identified after this time. To date, there has been limited use of wider immunisation around contacts.
‘Ring immunisation’ (to all around cases) was crucial for smallpox eradication. We propose consideration of a targeted ring strategy using digital tools to focus on the unvaccinated in communities with a new measles case. For example, the Aotearoa Immunisation Register (AIR) could be used to identify a wider ring of susceptible individuals in communities with cases, to whom immunisation could be offered. And more immunisation promotion and services nationally, with every case.
What this Briefing adds
- Despite growing concerns about the risk of a measles epidemic and calls to improve immunisation coverage, there has been limited change since our February Briefing.
- The number of susceptible children is now close to that before the 1980, 1985, 1991 and 1997 measles epidemics. Compared to those years, we now have more susceptible young adults, and hence may be primed for a large epidemic.
- Measles immunity in the primary school population limited spread in the 2019 epidemic; but with immunisation coverage low for those born since 2016 (8-year-olds and younger), that protection is largely gone.
Implications for public health policy and practice
- Catch-up MMR immunisation is urgently needed in addition to raising routine coverage. We have the tools, we just need policy direction and staff time to achieve high coverage in the priority settings of primary schools and pre-schools.
- Travel advice, and the processes for delivering it, need to be updated immediately to reduce the risk of travellers returning with the virus.
- The public health response to new measles cases could include more ‘ring immunisation’ in and around a community with measles cases; those susceptible could be reached using digital tools.
Author details
Dr Oz Mansoor, Medical Officer of Health, Tairāwhiti (on sabbatical with Public Health Communication Centre)
Prof Nikki Turner, Department of General Practice and Primary Care, University of Auckland, and Medical Director of the Immunisation Advisory Centre
Prof Nick Wilson, Department of Public Health, University of Otago Wellington, and Public Health Communication Centre
Dr John Kerr, Department of Public Health, University of Otago Wellington, and Public Health Communication Centre
Prof Michael Baker, Department of Public Health, University of Otago Wellington, and Public Health Communication Centre
Appendix 1: Measles immunity gaps and epidemic threshold
History of measles epidemics
Epidemic threshold calculated for 1979-1997 period
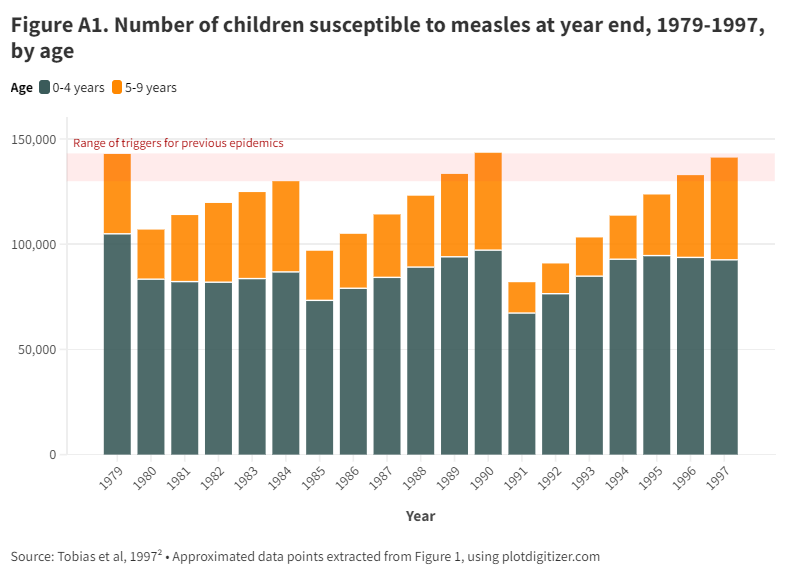
In 1996, we calculated the number of susceptibles that triggered previous epidemics in 1980, 1985, and 1991 (Figure A1). We found a threshold of around 130 to 140 thousand susceptible children aged under 10 years for an epidemic.
We had already breached the lower threshold in 1996. The calculation of susceptibles focussed on children aged under 10 years for data reasons. The recommended catch-up programme was for those under the age of 11 years.
In the subsequent epidemic, those aged 11 to 16 years had the lowest incidence rate among those aged under 30 years in 1997.2 This was the cohort that had received a second dose, delivered at school with good coverage.
Number of susceptibles in 2024
It is important to remain aware that immunity gaps are not uniformly spread across the community. These calculations do not address the variations. Clusters of low coverage increase epidemic risk.
To estimate child susceptibility, we obtained MMR coverage data by 3 age groups (1-4; 5-12; and 13-17 years), and from this calculated the % susceptible to measles assuming 90% and 99% vaccine effectiveness for 1 and 2 doses, as we did in 1996. And multiplied by the size of the population from Stats NZ as at end of 2023.
We also calculated those immune from disease, using notification data. As can be seen in Table A1, this adjustment adds little to estimated population immunity. Even if we multiplied by a factor to reflect under-ascertainment, it would also make little difference to estimates of overall susceptibility
Table A1. Calculating the immunity and implied reproduction number in 2024, by age group
| Coverage | Disease | Susceptible | |
| Age | Number | MMR*2 | MMR*1 | % Immune | Cases | % | % | Number | Re |
| | N | a | b | c= (a*.99)+(b*.9) | d | e= d/N | f=1-(c+e) | f*N | f*12 |
| 0y | 57,170 | 0 | 0 | 50.0% | 0 | | 50.0% | 28,585 | |
| 1-4y | 245,190 | 77.0% | 7.9% | 83.3% | 257 | 0.10% | 16.6% | 40,592 | 1.99 |
| 5-12y | 529,290 | 88.1% | 3.9% | 90.7% | 500 | 0.09% | 9.2% | 48,570 | 1.10 |
| 13-17y | 339,750 | 84.3% | 5.5% | 88.4% | 426 | 0.13% | 11.5% | 38,961 | 1.38 |
MMR*2 = receipt of both doses; MMR*1= receipt of one dose. Re = effective reproduction number.
Total susceptible children: 0-17y = 156,708; 0-12y = 117,747
We calculated the effective reproduction number (Re) by multiplying R0 by the % susceptible. For R0, we used 12 which is at the lower end of quoted range of 12-18 for measles, to be conservative. Rewas >1 in all groups, showing the potential for spread now.
In the above table we used the 1996 assumption that infants are fully protected until age 6 months and then fully susceptible until they are vaccinated. Infants are protected for the first months of life by maternal antibodies. As these are lower for mothers with vaccine-derived than disease-derived immunity, and there are now more of the former, this calculation under-estimates the numbers of under-1s who are susceptible.
The data provided by the MoH was not by number of doses, but ‘full’ or ‘partial’ immunisation. This is the same as 2 and 1 doses, respectively. Except for children aged <15 months, where being “fully immunised for age” is a single dose. This means some under-estimation of the number of susceptible in the 1-4y age group.
Unlike 1996, we did not model the impact of disease immunity as there has been limited disease since 1997: 4,020 notified cases from 1998 to 2023, half of whom (n=1932) were born from the year 2000. For the age group of most concern, those born from 2016 there were 531 notifications. Assuming only half the cases were notified that reduces the number susceptibles in this age group by 1000.
The measles immunity age profile has changed considerably since 1997, with more susceptible young adults. We now have nearly 40,000 children aged 13-17 years who are susceptible, in contrast to a highly immunised cohort aged 11 years and over in 1997.
So, while we cannot directly compare the 2024 to the 1996 calculations, we now have at least 156,708 susceptible children aged under 17 years, of whom 117,747 are aged under 10 years, compared to the 130,000 susceptible threshold children aged under 10 years we found in previous epidemics.
All these points make it hard to say how close we are to the epidemic threshold (or if it has already been passed), but as we have seen in our analysis of Re, this is over 1 in all groups nationally, and will be even higher in some communities.
Immunity profile from disease data
A 2017 risk assessment that used a serosurvey and case data concluded that “overall population immunity against measles remains borderline (about 90%) and is lower in those born between 1982 and 2005 (approximately)”.5
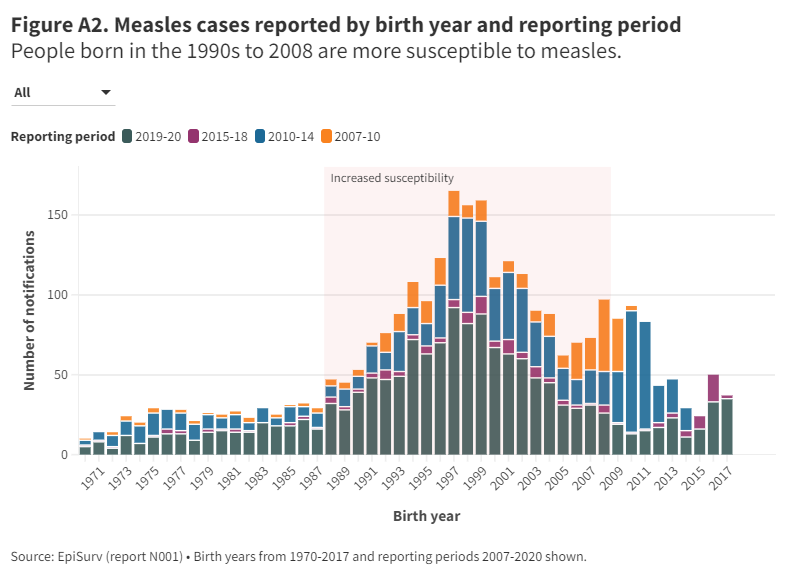
Using notification data from the national database (EpiSurv) we can infer immunity gaps by birth year (Figure A2). For those born from 1988 to 2008, the larger number of cases can be seen for all time periods, with most data coming from 2019-2020, ie, reflecting current susceptibility patterns.
The progressive decrease in 2019-20 cases from the 2000 to 2010 birth cohorts reflects the progressively improving coverage, so lower susceptibility. More cases in those born from 2010 in the 2019-20 notifications likely reflect the increase in cases in youngest children with the highest rates in under-2-year olds (the 2018 and 2019 births had the most notifications in 2019-20, and are not included in Figure A3)
The notifications from every time period imply an increasing immunity gap until 1997/8 that then decreases to about 2010. Figure 1 also highlights the size of the 2019 epidemic, with more notification than all notifications from 2007 to 2018; there were measles outbreaks in 2009, 2011, 2014, 2016 and 2019.
A 2014 national serosurvey, the latest available, found overall 13% non-immune and 10% equivocal. Accepting the equivocal results as being immune this suggests well over half a million susceptibles. The survey found 1%, 3 to4%, and 16% measles-susceptible in those born before 1962, from 1962 to 1990, and 2001-2007 birth cohorts (highest), respectively.
Change in hospitalisation over time
Over a third of known cases were hospitalised in 2019,6 compared to 14% in 1997 and an estimated 1-2% in 1991.2 The increase over time may reflect a trend, as well as the change in age profile of cases. It does suggest the risk of a greater health system burden in future measles outbreaks.
Appendix 2: Border measures to reduce risk of measles virus entry
The importance of border measures
It does not matter how many susceptible children there are, if the measles virus is not brought into the country: we will maintain our measles elimination status. We outlined some suggestions in our earlier Briefing (travel requirements, documentation of measles immunity, including migrant immunisation status on the Aotearoa Immunisation Register (AIR), and airplane wastewater surveillance). Of these official travel advice can be rapidly implemented for little cost.
Who needs travel advice?
The primary risk from travel is probably not from visitors but returning residents. In the USA, 62%, 77%, and 63% of imports were from residents in 2001-2016,7 2019,8 and 2020-March 2024,9 respectively. For Australia, 60% of imports were from holidays, with most of them visiting friends and families.10 All three measles imports in 2023 in NZ were from returning travellers.
So, travel advice is needed both for residents leaving NZ for, and for visitors coming from, any country with current spread of measles. Both groups could be advised as part of the travel booking process. At present, much of the world is affected, and it would be appropriate to give to all travellers, given that exposures in airplanes could also affect travellers going to measles-free areas.
For visitors, another option could be made available as part of the NZ travel declaration (NZTD). Additionally, the NZTD could be requested on departure for residents.
Travel advice
For residents booking travel from NZ, the government could request inclusion of a question on measles immunity as part of the travel booking. To minimise cost and maximise compliance, the process needs to be integrated with required government processes, such as the NZ Travel Declaration. However, as this declaration is required for entry, not exit, a prompt on the importance of measles vaccination could be included in the travel booking.
Rather than making it a legal requirement, developing IT systems that facilitate compliance are likely to be more acceptable and effective, and avoid unnecessary regulation - a current government priority. But this approach could be reviewed in the situation of a large measles epidemic in a country with strong travel links to NZ, as we have seen with the Philippines for example.
A low-cost option that could be immediately implemented is to update the official travel web sites with messages to:
- Check if you are immune to measles, as the global risk of measles is on the rise.
- If you do not have documented immunity to measles, get the vaccine at least two weeks before you travel. (In NZ, you can get the vaccine from your general practice free of charge).
- Obtain and travel with documentation to show immunity, in case you become a measles contact to avoid quarantine on your return to New Zealand.
- Where to get more information on measles disease and MMR vaccine.
Other measures
Identifying people who bring measles into the country could be prompted by wastewater surveillance on aircraft, but would require additional work to identify the person. And setting up a testing programme that would be logistically complex and somewhat resource intensive. Nevertheless, the concept is worth exploring as part of national wastewater surveillance of a range of infectious risks, given its value for Covid-19 surveillance.
Health screening upon arrival (and departure) could be included as part of travel documentation. This process would require additional staff time to operate, and follow-up of those who responded positively to screening questions. Alternatively, the data could be shared with the local Medical Officer of Health for follow-up, as appropriately. Again, additional resources would be needed.
Given the importance of border measures to limit or stop introduction of measles virus and other infectious threats, including a future pandemic, a broader review is urgently needed. A wide range of possible measures, including legislated requirements and the use of the NZ travel declaration, need time to carefully deliberate so need to start soon.